Abstract
Introduction: Sickle Cell Disease (SCD) is characterized by chronic inflammation with innate immune cell activation, especially observed in neutrophils. Emerging evidence implicates the imbalance between neutrophil extracellular trap (NET) formation and degradation as having a central role in the pathophysiology of thromboinflammation and venous thrombosis. Although NETosis and NET formation influences venous thromboembolism (VTE) pathophysiology, little is known about baseline and agonist-induced NETosis in SCD. We hypothesized that systemic neutrophil activation would lead to higher baseline and agonist induced NETosis in SCD and would influence phenotypic variability. To test this hypothesis, we assessed baseline and agonist induced NETosis in patients with SCD and ethnic matched controls. We also investigated the anti-inflammatory effects of flavonoid Quercetin on neutrophil activation.
Methods: Neutrophils negatively selected from citrate anticoagulated blood using an immunomagnetic bead based kit (MACSxpress® Miltenyi Biotec) were either fixed immediately to assess baseline NETosis or stimulated with fMLP (1 µM) for 1 hour to assess agonist-induced NETosis. To study flavonoid anti-inflammatory effects, neutrophils were pretreated with Quercetin (100 µM) for 30 min prior to fixation and fMLP stimulation. NETosis was assessed by flow cytometry. Extracellular DNA extrusion on neutrophils was detected by gating the neutrophil population staining with Sytox green. Sytox green positive neutrophils that were positive for both myeloperoxidase (MPO) and tri-Citrullinated Histones (H3Cit) were defined as undergoing NETosis. In some experiments, NET formation was independently confirmed by image flow cytometry (AMNIS).
Results: Subjects included SCD patients (genotype SS n=11) and ethnic matched controls (genotype AA, n=11) with a median age of 49 years (p=0.58) and a predominance of males (70%). All SCD patients were at least 60 days remote from an acute painful vaso-occlusive crisis or blood transfusion and were receiving hydroxyurea. The white cell and absolute neutrophil counts were higher in SCD patients (mean ± SD 8.77 ± 1.52 and 5.07 ± 1.78 x 10 9/L) when compared with controls (mean ± SD 5.33 ± 1.05 and 2.8 ± 0.95 x 10 9/L). Subsequent data are presented as median percentages with interquartile ranges (IQR).
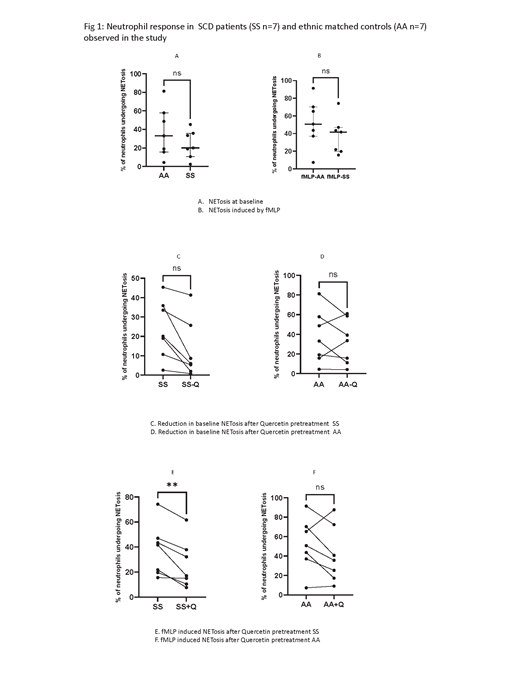
A subgroup of the study population demonstrated spontaneous NETosis (27%; SS = 4; AA = 4) and were therefore excluded from our analysis. Contrary to expectations, SCD patients exhibited a lower percentage of NETosis at baseline compared to controls (20 % (11, 36) vs. 33 % (15, 58); p=0.22). Similarly, neutrophils from SCD patients exhibited lower agonist-induced NETosis compared to controls (42% (19, 47) vs. 51% (37, 70); p=0.15) (Fig 1 A and B)
Pretreatment of neutrophils from SCD patients with Quercetin appeared to inhibit basal levels of NETosis (6%, (2, 26) vs. 20% (11, 36) p=0.08) although this effect was not appreciable in controls (33% (11, 58) vs. 33% (15, 58) p=0.41) (Fig 1 C and D). Neutrophils from SCD patients that were pretreated with Quercetin and then stimulated with fMLP demonstrated significantly reduced NETosis compared to untreated neutrophils (17.1% (10, 38) vs 41.7% (19, 47) p=0.007) although this effect was not significant in controls (35% (17, 72) vs 50.7% (37, 70) p=0.11) Fig 1 E and F.
Our ongoing experiments will demonstrate the effects of more specific inhibitors of neutrophil activation (e.g. R406) in human and mouse models of SCD.
Conclusion: These preliminary data suggest lowered NETosis in SCD patients despite neutrophil activation in the systemic inflammatory environment that are partially explained by hydroxyurea treatment. The results also support further evaluation of anti-inflammatory therapies to reduce neutrophil activation in SCD and ameliorate thrombo-inflammatory disease pathology.
No relevant conflicts of interest to declare.